Laparoscopic Biliopancreatic Diversion with Duodenal Switch
How it works:
The Biliopancreatic Diversion with Duodenal Switch is both a restrictive and malabsorptive procedure.
The duodenal switch can be performed laparoscopically and is the most extreme procedure done today for weight loss. It is a more complex surgery and is usually reserved for those patients with a BMI over 55. (see figure) The restrictive component involves reducing the size of the stomach. The surgeon would divide the stomach vertically and remove more than 85 percent of it. The stomach that remains is shaped like a banana. Duodenal switch surgery is a variation of another procedure, called biliopancreatic diversion. But the duodenal switch leaves a larger portion of the stomach intact, including the pyloric valve, which regulates the release of stomach contents into the small intestine. As the name suggests, the duodenal switch also keeps a small part of the duodenum in the digestive system. The duodenum is the first part of the small intestine. It is located between the stomach and the jejunum, or the middle part of the small intestine. Unlike the Roux-en-Y gastric by-pass, which employes a gastric “pouch” and bypasses the pyloric valve, the DS procedure keeps the pyloric valve intact. This eliminates the possibility of dumping syndrome, marginal ulcers, stoma closures and blockages, all of which can occur after other gastric bypass procedures.
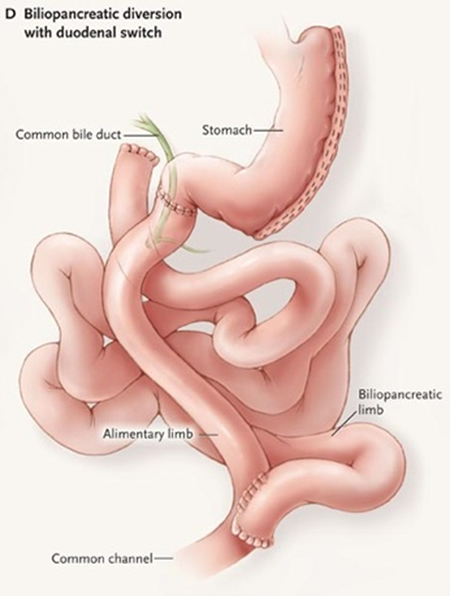
Malabsorptive surgeries restrict the amount of calories and nutrients the body absorbs. The malabsorptive component of duodenal switch surgery involves rearranging the small intestine to separate the flow of food from the flow of bile and pancreatic juices. The food and digestive juices interact only in the last 18 to 24 inches of the intestine, allowing for malabsorption. Unlike the restrictive part of the surgery, the intestinal bypass part of the duodenal switch is partially reversible if you are one of the people who experience malabsorptive complications.
What to expect after surgery:
Part of the recovery process involves getting re-accustomed to eating solid foods. People who undergo the duodenal switch can consume only fluids immediately following surgery. From there, they will progress to pureed foods and ultimately solids.
Most of the weight loss with the duodenal switch occurs during the first 12 to 18 months after surgery. With this procedure the patient should expect to loose about 80 to 100% of excess body weight.
The duodenal switch may result in more nutritional deficiencies than other weight loss surgeries because of the malabsorption it causes. As a result, the patient will need to take nutritional supplements, including vitamin A, vitamin D and calcium, daily for the rest of his/her life. Some doctors may also recommend additional supplements of potassium and iron. Lifelong nutritional follow-up is needed after duodenal switch.
There are other nutritional considerations after undergoing duodenal switch. For example, eating fatty foods tends to cause foul-smelling gas and diarrhea. In addition, some very starchy foods may cause gassiness. Note that everyone responds differently to different foods, so every patients experience varies.
All surgeries have short- and long-term risks. The short-term risks of duodenal switch include:
- Bleeding/blood loss
- Blood clots
- Infection
- Leakage. A leak means that a perforation of the stomach or a leak from anywhere the bowel is stitched together has occurred.
The long-term risks of duodenal switch include:
- Nutritional deficiencies
- The brittle bone disease osteoporosis, due to malabsorption of calcium and vitamin D, which are needed to maintain bone strength
- Night blindness due to malabosption of Vitamin A
- Malabsorption of protein, leading to malnutrition. This may lead to a second operation.
- Carbs can be well absorbed, resulting in inadequate weight loss
- Chronic diarrhea. Patients may have many loose bowel movements in a day. In the duodenal switch, the surgeon shortens the amount of bowel that the food goes through and diverts the digestive juices. The food goes through half of the intestines and then does not meet the digestive juices until the tail end of the intestines. This cripples the digestive process, resulting in diarrhea.
- Foul-smelling stools and gas
Compared with other types of weight loss surgery, the duodenal switch has these advantages:
- The remaining stomach is much larger after duodenal switch surgery than following gastric bypass; this allows for larger meals.
- Reduced risk of developing ulcers
- The intestinal bypass part of the surgery is partially reversible for those having malabsorptive complications.
- Possibly greater long-term weight loss and less chance of regaining weight
- More rapid weight loss, compared with gastric banding procedures
- Lower risk of dumping syndrome, which occurs when the undigested stomach contents are “dumped” into the small intestine too quickly. It is marked by abdominal cramps and nausea.
- Regression of obesity-related illnesses
Long Term Results:
Based on patient averages, one can expect to lose about 80 to 100 % of the excess body weight. Lifelong nutritional follow-up is mandatory.
Relevant Articles Published by Dr. Frantzides on this Procedure
Minimally Invasive Biliopancreatic Diversion with Duodenal Switch;
In Atlas of Minimally Invasive Surgery Frantzides CT, Carlson (eds.) Elsevier 2008.
Want to Know More About Dr. Frantzides? See what others are saying: www.ObesityHelp.com
